Country focus: Nigeria
Theme: antenatal care
Authors: Zainab Mohammed, Mukhtar Sani, David Adeyemi, Olufunke Fasawe
Author affiliation: Clinton Health Access Initiative (CHAI)
The problem
In Kano, 51% of pregnant women attended the recommended 4 Antenatal Care (ANC) visits, compared to national averages of 57% (2018 NDHS). Skilled birth delivery coverage is 21.5%, 23.2% of mothers received postnatal services, and 34% of pregnant women received at least 2 doses Intermittent Preventive Treatment of Malaria in pregnancy (2018 NDHS).
The context
Group ANC (G-ANC) is a tested, alternative model to traditional ANC, considered to be potentially more effective in driving women to complete a full cycle of antenatal care visits than traditional service delivery. The approach is designed to integrate all pregnancy-related health assessments and motivate behavioral change among pregnant women and Healthcare providers.
In brief
CHAI with support from Technical Advice Connect, provided technical assistance to the Kano State Primary Health Care Management Board to deploy and sustain G-ANC in 484 health facilities across all 44 Local Government Authorities in Kano State.
Using responsive feedback, the team modified program design to overcome two core limitations, gestational age eligibility restrictions and session content, which were hindrances to success in the Kano context.
Aligning stakeholders on key concepts
At the outset, program stakeholders (the CHAI team, KSPHCMB, and Ministry of Health) defined the G-ANC method and reviewed expected outcomes, based on a pilot study from another state. To translate the pilot model to the Kano context, stakeholders replicated key program designs. Firstly, the gestational age for eligible pregnant women was 16-20 weeks, and secondly that the RMNCH messaging for ANC were structured by 8 sessions.
The implementation approach set out mentoring sessions for master trainers, who would then train and supervise healthcare provides, observe grassroots nuances and report on any issues with uptake.
Seek evidence
Responsive Feedback mechanisms were defined by stakeholders with the aim of prioritizing local ownership, to affect community-level change:
- Quarterly client exit interviews on the quality of service
- Desk review of facility performance data to monitor progress towards achieving program goals
- Convening of stakeholders to reflect on findings and modify program approaches
Data collected showed low enrolment of women in G-ANC cohorts after the first phase of implementation. This prompted a review of processes by key stakeholders.
The session reviewed data in light of the key learning question: How is the current criteria limiting the enrolment of pregnant women and coverage of RMNCH counselling at ANC clinics?
How evidence informed program evolution
Data highlighted how program design was inappropriate for the Kano context.
- Clients were not reporting early enough to be eligible for sessions, when gestational age limits were set to 16-20 weeks; 75% of women enrolling were above 20 weeks.
- Coverage of women who received counselling were below optimal. The counselling structure of one-topic per visit was not appropriate; women enrolling late would miss crucial sessions or would not have a holistic understanding of the value of the course.
- High volume facilities did not have the resource to conduct RMNCH multiple sessions concurrently.
In light of these findings, the below changes were made to the program:
- Gestation limits were removed
- An abridged messaging course was created, and a summary session of ANC visits 1-8 was introduced to start each session
- Assigned flexible schedules for cohorts, such as giving time slots for high-volume facilities. For low-volume facilities, the CHAI team are currently exploring whether to group women by the number of children they have as well as gestational age, to make up the standard number of pregnant women per cohort and nurture peer learning opportunities.
- A further amendment was the intensification of male involvement counseling by service providers and community influencers, to invite partners to accompany and encourage their spouses at the RMNCH sessions.
Outcomes
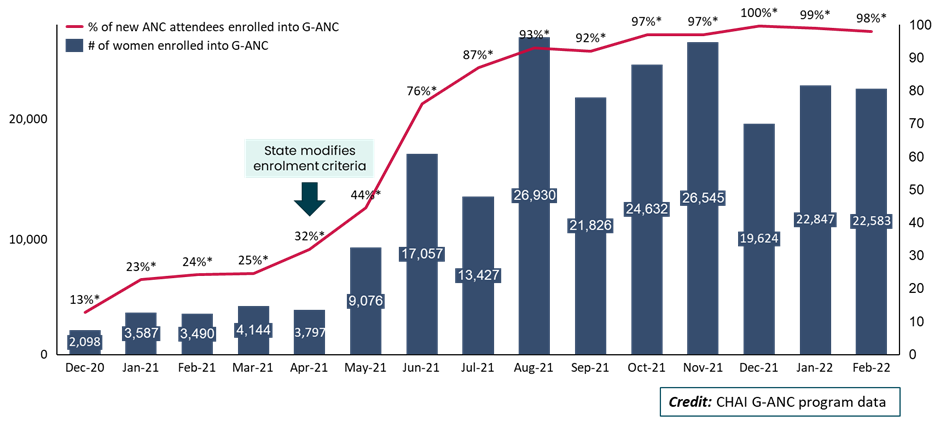
Following enrolment modifications, an increase in the influx of PW accessing G-ANC services was observed, with 221,663 PW enrolled into 18,406 G-ANC cohorts, and this accounts for a 6-fold increase of ANC new attendees enrolled into G-ANC from 13% in December 2020 to 98% in February 2022.
As well as enrollment to G-ANC, there was also an increase in coverage of women counselled on RMNCH services. Pregnant women received the modified counseling during every ANC visit.
Although the summary session was introduced to give women a more in-depth understanding of the benefit of the course as a whole, an unintended positive outcome of this was that women from these cohorts became champions of ANC services in their social circles and encouraged others to attend each session. Therefore, it provokes word of mouth which improved attendance.
With the programmatic changes it has been possible to integrate G-ANC into existing policies. This program achieved major changes to policy. Furthermore, the Kano State Primary Health Care Management Board has adopted G-ANC into the healthcare budget which commits to using one PHC per ward to improve access to services.
Lessons learned
- Periodic feedback from clients helps to enhance interventions to suit clients’ needs and yet maintain fidelity of the interventions.
- When used to guide program implementation, responsive feedback increases sense of ownership, and promotes sustainability with improved stakeholder involvement.