Country-focus: Nigeria
Theme: Family Planning
In brief
Clinton Health Access Initiative (CHAI) uses responsive feedback to continuously iterate the design of their Post-Pregnancy Family Planning (PoPCare) program to increase the availability of IUD instruments and the motivation of healthcare providers to counsel young first-time mothers on these methods.
Program context
The goal of the Clinton Health Access Initiative’s (CHAI) Post-Pregnancy Family Planning (PoPCare) program is to increase access to, and uptake of, modern contraception methods post-pregnancy, particularly among young first-time mothers. The program seeks to increase uptake of family planning among women who have given birth outside a health facility with a focus on first time mothers. The program is implemented in 11 Local Government Areas (LGAs) in three states namely Lagos, Nasarawa and Rivers.
To achieve this goal, the PoPCare program trained traditional birth attendants (TBAs), Community Health Extension Workers (CHEWs) and community volunteers (CVs) to advise young women and new mothers on modern contraception. This included referring them to health facilities where they could then obtain a family planning method of their choice, from PoPCare trained health care providers.
How they used responsive feedback
Findings from a 2019 baseline facility survey showed that many providers at health facilities lacked the motivation or ability to provide IUD insertions, hence the team needed to understand the causes.
To address these issues, the PoPCare team conducted two waves of a rapid assessment survey among a sample of health care providers and made program adjustments based on the findings of each wave of data. In each project state, one fairly typical LGA was selected, and within each of those LGAs a convenience sample of 10-20 health care workers were interviewed using a short structured questionnaire.
Findings from Wave 1
The data collection for Wave 1 took place between March-June 2020. The findings showed that, due to personal beliefs about family planning use, numerous providers felt embarrassed and found it hard to counsel young first-time mothers about the benefits of family planning. The motivation varied considerably by state, with health workers in Rivers state being more motivated than those elsewhere. Additionally, many reported that they felt ill-equipped to insert IUDs and advise on their potential side-effects.
Program adjustments following Wave 1
To improve provider’s confidence when counseling, the PoPCare team included additional training sessions on FP counseling and IUD side-effect management in the clinical mentoring component of their program. These training sessions were adjusted to include modules on values, clarification, and attitude transformation so that providers felt confident having conversations regarding family planning and cultural values. For example, Health care workers received a values clarification and attitude transformation (VCAT) training exercise alongside their Post-Pregnancy Family Planning training so they can offer unbiased services to clients particularly YFTMs.
The program also improved providers skills and ability to perform IUD insertions, by running refresher training and mentoring sessions that included practice sessions on pelvic models and live clients.
Findings from Wave 2
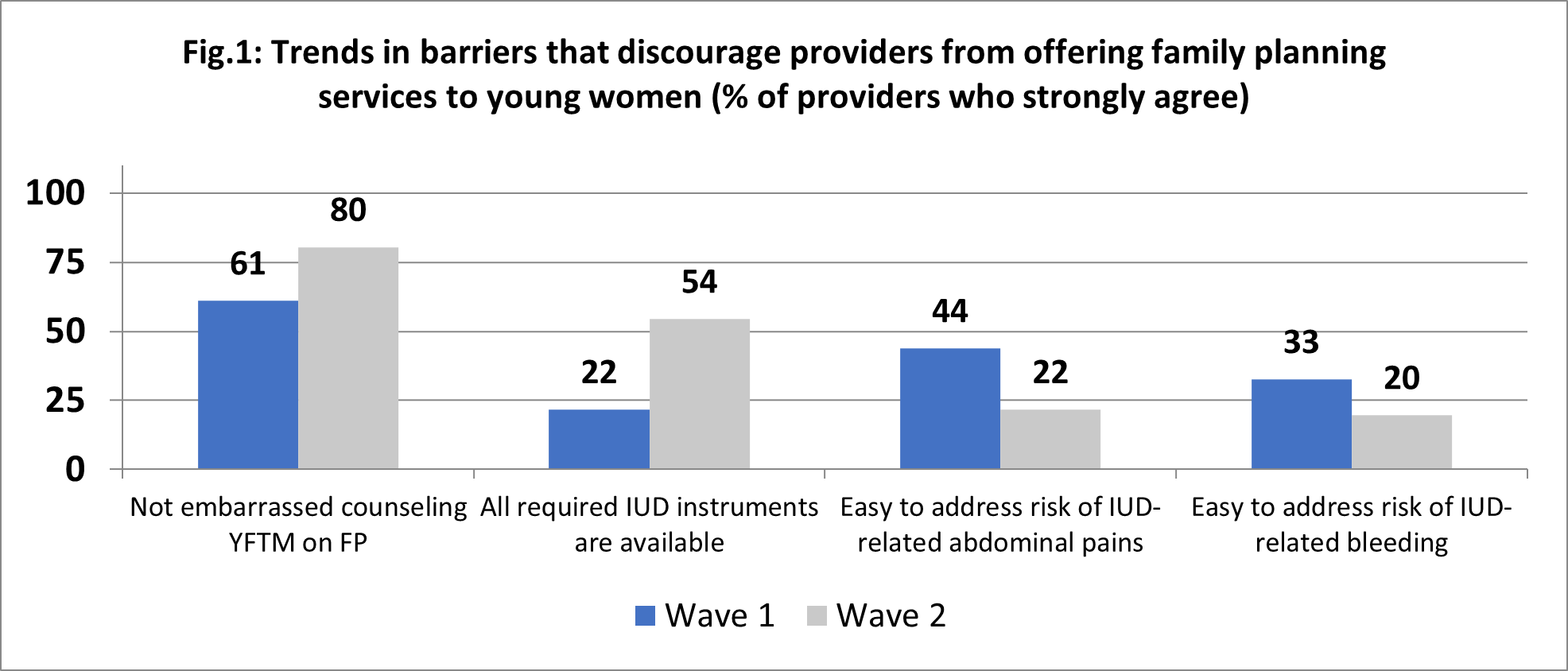
The data collection for Wave 2 took place between November-December 2020, following the first round of program adjustments. The data showed the program adjustments made from Wave 1 had the following outcomes:
- A higher percentage of providers did not feel embarrassed counseling young first-time mother about modern family planning. Confidence grew from 61% at Wave 1 to 80% at Wave 2.
- There was a notable improvement in the percentage of providers who reported that all required IUD instruments were available in their facility. Availability increased from 22% at Wave 1 to 54% at Wave 2.
However, Wave 2 data also showed further room for improvement:
- As rates of access remained low – around 54% – further improvements were needed to ensure that IUD instruments were readily available and easy to access.
- Unfortunately, the training sessions on the management of IUD side-effects did not have the desired effect, and provider confidence in managing IUD side-effects had further decreased.
Overall results
To learn how these programmatic tweaks had affected overall IUD uptake, the team compared routine data collected on a monthly basis. To make each of periods comparable, the team looked at data collected within a 3-month period following the survey and program adjustments. Figure 2 sets out the periods of data collection which took place across:
- Jan-March 2020 – before programmatic adjustments
- July-Sept 2020 – following programmatic adjustments from the Wave 1 survey
- March-May 2021 – following the second series of programmatic adjustments after the Wave 2 survey
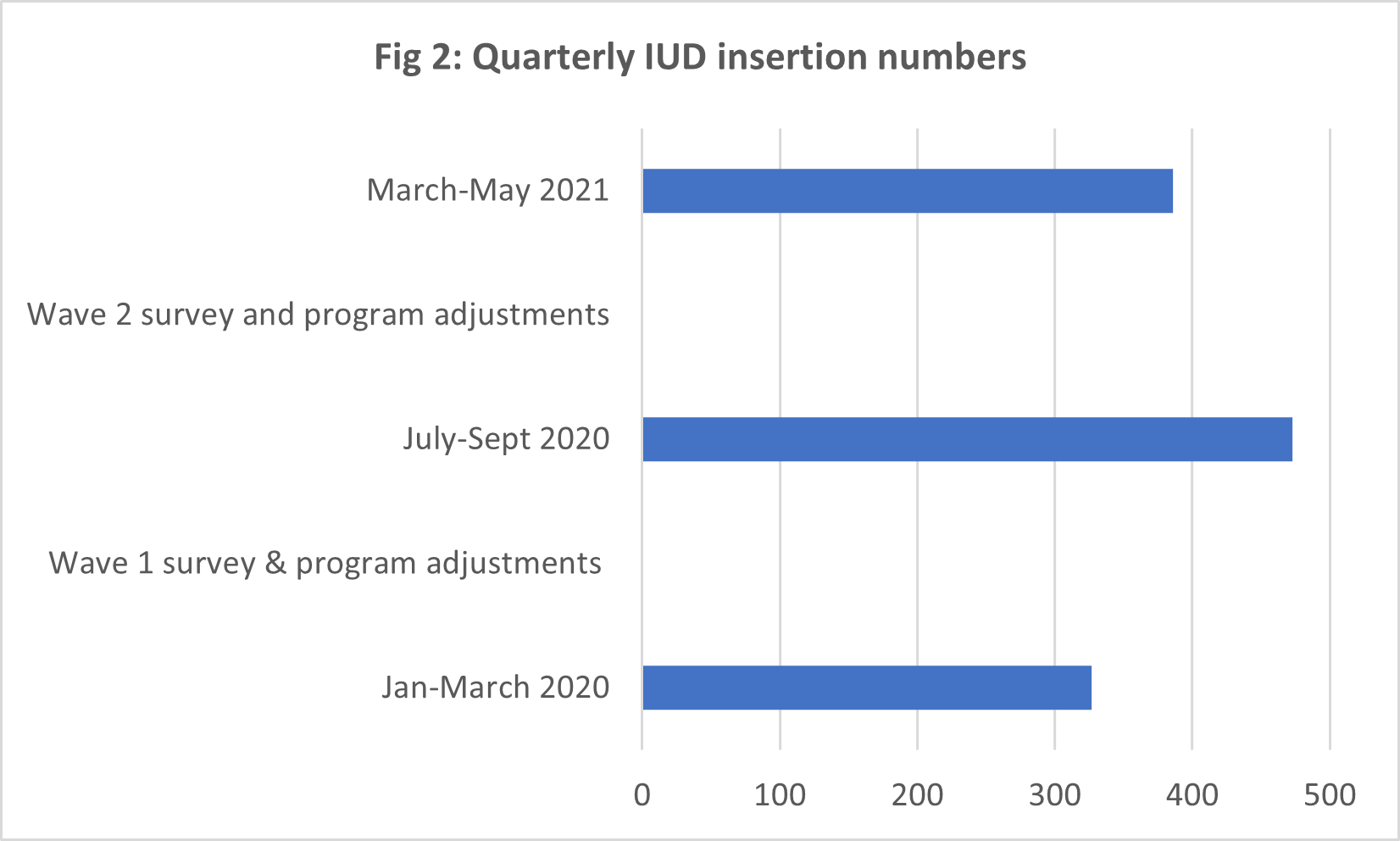
The findings showed that:
- The programmatic adjustments made following Wave 1 led to an overall improvement in IUD insertions over a 3-month period from 327 in Jan-March 2020 to 473 in July-Sept 2020.
- However, IUD insertions declined to 385 in period March-May 2021, following the tweaks made after the Wave 2 data collection. This decline was likely linked to a COVID-19 lockdown in some program states (Lagos and Rivers) which affected access to family planning services at the program supported health-facilities.
The growth in provider confidence at Wave 2 confirmed the positive impact of the additional training sessions integrated at Wave 1. These modules will be retained in future trainings given to family-planning providers (including refresher trainings). The PoPCare team plans to initiate Wave 3 of the rapid assessment surveys to assess the effect of these latest program adjustments following findings from Wave 2.
Lessons for others
- Progress is not linear: As IUD insertions data showed, progress is changeable. Responsive feedback enabled the PoPCare team to identify declines early on, and continue to adapt their program in light of new learnings.
- Small studies can yield big lessons. Small samples can still provide a lot of information. These insights can be useful for making program course corrections in between bigger studies.
- MEL teams and program implementers make a good team. MEL teams can detect patterns and anomalies in feedback, and implementers can interpret the feedback in context. Regular review of program data and previous RFM data by MEL and program teams provides a good context for institutionalizing responsive feedback mechanisms.
- Feedback helps you see the real reasons instead of making assumptions. The persistently low levels of IUD instrument access were an unexpected finding for the PoPCare team. The feedback prompted the PoPCare team to conduct service readiness assessments (SRAs) to determine whether the instruments donated by the program needed to be replenished, or whether there was merely a need to better manage access within the facilities.
Authors
- Nneka Onwuasor, Clinton Health Access Initiative Nigeria
- Rosemary Ayu, Clinton Health Access Initiative Nigeria
- Owens Wiwa, Clinton Health Access Initiative Nigeria
- Olufunke Fasawe, Clinton Health Access Initiative Nigeria
- Dominique Meekers, Tulane University
FIND OUT MORE
To find out more contact Nneka Onwuasor on nonwuasor@clintonhealthaccess.org