Author: Dr ‘Layi Olatawura, Health Strategy and Delivery Foundation (HSDF)
Country focus: Nigeria
Theme: Data for decision-making
In brief:
Kaduna State had low quality routine data, inhibiting their ability to make informed decisions and improve service delivery in primary healthcare facility. As part of the BMGF-funded primary healthcare transformation program, Shugabanci, HSDF created data control rooms to address this issue and improve evidence for decision-making.
Problem and context:
The Shugabanci Program (a project of the HSDF Health Systems Strengthening Unit) worked with key development partners and stakeholders in 2017 to strengthen primary healthcare in Kaduna State. The focus was on the development and delivery of Governance, Supply and Demand interventions through the provision of direct support to Kaduna State’s Primary Healthcare Development Agency (SPHCDA), the State Ministry of Health and related MDAs. These interventions were in four key areas: Service Delivery, Financial Management, Organizational Capacity Management, and Human Resources for Health.
Kaduna state already had delays in data reporting; a lack of robust, routine data meant the state relied on survey data to make key decisions on service delivery. These surveys occurred infrequently (roughly every 4 or 5 years), and each was very limited in scope.* Moreover, the service delivery data was very poor in availability, validity, and consistency. Despite significant government investment and donor support, key indices remained suboptimal.
Overall, this meant that there was not enough visibility of routine health facility and community service delivery performance, which hindered the state’s ability to address service delivery issues in a timely manner. It became necessary to address how high quality and regular data could be retrieved from the DHIS 2 – a monthly routine data survey – for decision making
An Integrated Data Control Room (IDCR) was created to strengthen the quality of monthly reported data from health facilities
In order to strengthen the quality of monthly reported data from health facilities, the team created an Integrated Data Control Room (IDCR). This was a physical room to track data quality each month. There were four key steps in its inception:
- Identify key stakeholders and select indicators. The team mapped out multi-level stakeholders, involved in data management and healthcare service delivery, and emphasized to them the need for credible data for decision-making. Together with these stakeholders, they shortlisted priority indicators within programmatic areas. Kaduna state’s IDCR currently track indicators across 5 thematic areas: RMNCH, Immunization, Malaria, HIV, and IMCI.
- Capacity building. The team ran capacity building workshops on how to identify data reporting issues (quality, timeliness, completeness) on the DHIS 2. These workshops involved program leads and M&E officers who were put in touch with data focal personnel. Together, they developed data validation rules to checks for errors.
- Location and schedule. The team selected a physical location and specific time to review incoming data – this was the ‘data room’. For priority facilities with particular challenges, the team conducted follow-up quality check correction and mentoring visits. For example, in Kaduna state, the data control room sessions are conducted every 3rd week of the month, with follow-up facility correction visits taking place the following week.
- Tools & templates development. The team also designed simple Excel templates for identification of errors using defined ‘data validation rules’ and tracking of corrective actions.
What did the evidence reveal?
The IDCR process adopted an adaptive and iterative process, with extensive health sector stakeholder participation. Some key highlights are below:
- More data quality checks required. Regular use of the validation rules and cross-referencing of data; expected trends revealed problems in other areas. To put it simply, the more issues addressed, the more gaps were revealed.
- Use of data to identify other health system issues. As well as the data quality gaps, it became clear that there were broader health system gaps: e.g. stockout rates in drug commodity supply, human resource capacity at multiple levels down to the facility.
- Insights on population access to services at the facility: coverage data enabled the state to identify populations in need of services across local government areas e.g. trends in PHC general attendance over periods.
- Progress with decisions made with initial IDCR results: Initial findings led to other interventions, like a Service Availability Mapping (SAM) across focal PHCs to further guarantee data credibility – this was a diagnostic to verify services that are actually being provided so that when data comes in, the data team can (i) ascertain whether the data is complete and (ii) track service provision.
What were the results?
Implementation of the IDCR commenced in Q3 2018 and resulted in a rapid increase in Kaduna State’s DHIS reporting rate. Before the implementation of the IDCR the reporting rate was around 70%, below the national target of 80%.
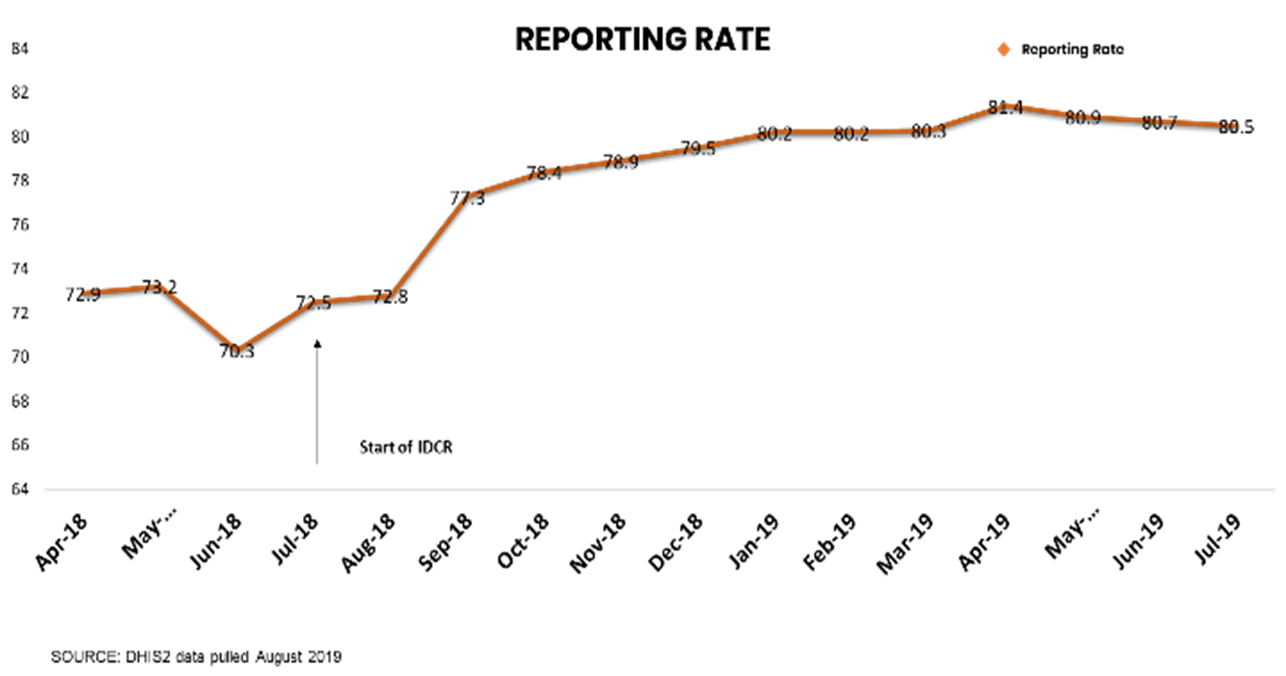
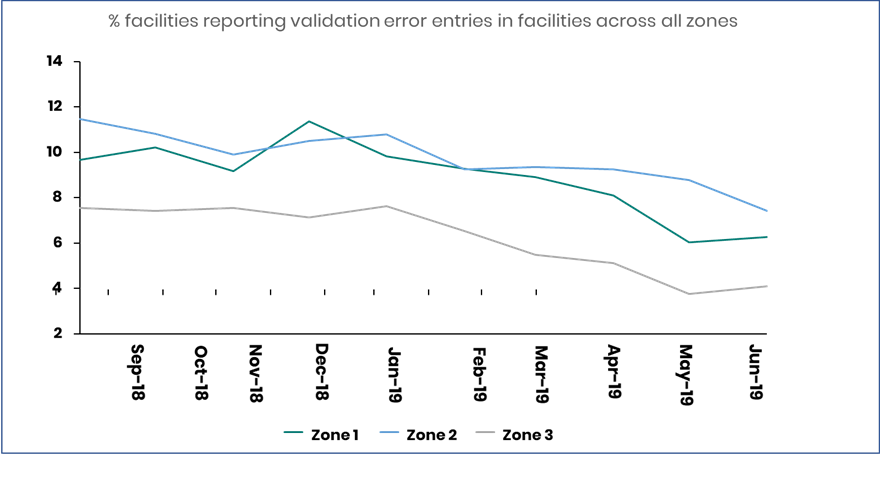
There was a corresponding reduction in data errors because of tracking errors From January 2019, the State IDCR team conducted facility and LGA follow-up visits to validate the reported NHMIS data. This further drove up data quality with <10% of the health facilities now reporting data errors.
Data quality improvement through the IDCR has influenced service delivery decisions and state health annual operational work plans
- Programmatic performance reviews have commenced, leading to corrective solutions within program areas such as RMNCAH.
- Human resources gaps, and the need for capacity building for data management ,and quality service delivery have been identified and improved.
- There has been institutional change on the need for data to make key decisions in the state. A Health Sector Monitoring and Evaluation framework has been used in the development of state health plans.
- Routine (quarterly) DHIS data analysis helps the state identify thematic areas in need of urgent focus (using scorecards); corrective interventions are developed, costed and included in state Annual Operational Plans for implementation.
Lessons for others on using data for making better decisions:
An integrated data control room is a simple intervention that can be deployed anywhere, leveraging already existing resources (like WhatsApp, phone calls and Excel spreadsheets) to create greater accountability for data. For easy deployment:
- Ensure that roles and responsibilities are clearly communicated to people responsible for data reporting.
- Identify opportunities to build staff skills and knowledge.
- Create a system that encourages healthy competition amongst staff. With the 23 data managers in Kaduna, competition tends to improve staff capacity.
- Staff can be recognized for improvements and compliance with small rewards, like the gift of internet data.
Where can I find more information?
Dr ‘Layi Olatawura: layi.olatawura@hsdf.org.ng
Aliyu Adamu Tsafe: aliyu.adamu@hsdf.org.ng
Dr Hamza Abubakar: hamza.abubakar@kdsg.gov.ng
*NHMIS: National Health Management Information System DHIS 2: Nigeria District Health Information System. NDHS: National Demographic Health Survey – 5 years. MICS: Multiple Indicator Cluster Survey – 4 years. NNHS: National Nutrition & Health Survey